Simply adding an anti-inflammatory medication to the antiviral already used to treat herpes encephalitis could potentially prevent lasting damage from the dangerous brain infection.
The challenge: About two-thirds of the population is infected with herpes simplex virus-1 (HSV-1), and most of the time, they don’t even notice — it’s only during the occasional flare up that they experience mild symptoms, such as cold sores.
Rarely, though, HSV-1 can infect the brain, causing herpes encephalitis, a serious neurological disorder with symptoms that include seizures, partial paralysis, and memory loss. There are about 2,000 cases in the US each year.
Herpes encephalitis is treatable with antiviral medications, such as UK drugmaker GSK’s acyclovir (ACV), but even with treatment, the disorder is fatal in 20-30% of cases, and those who do survive are often left with lasting neurological problems.
“Important experiments can be conducted with [these proto-brains] that were impossible a few years ago.”
Nikolaus Rajewsky
Mini brains: Developing more effective treatments for herpes encephalitis has been difficult because there isn’t a good animal model of the disease and getting samples of infected human brains for drug testing isn’t practical.
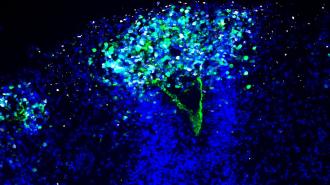
To overcome this issue, researchers at the Max Delbrück Center (MDC) in Germany created mini brains, or “brain organoids,” by coaxing stem cells into growing into tiny clumps of neurons.
“These proto-brains contain hundreds of thousands of neurons that can communicate with each other in a synchronized manner,” said senior author Nikolaus Rajewsky. “Important experiments can be conducted with them that were impossible a few years ago.”
The study: After making their organoids, the MDC researchers infected them with HSV-1 to see how it affected the various brain cells. This led to the discovery that the virus activates the “TNF-α signaling pathway,” a series of chemical reactions linked to inflammation.
Inflammation can help our body fight viruses, but it can also damage tissue. When the researchers treated their infected brain organoids with ACV, the herpes virus stopped replicating, but the TNF-α signaling pathway remained activated.
“When we block viral replication with antiviral drugs, the overzealous inflammatory response could instead become damaging.”
Tancredi Massimo Pentimalli
In their study, the researchers note that “sustained inflammation can be toxic to neuronal cells” and that this activity could explain why 70% of herpes encephalitis patients treated with ACV “do not completely recover neurological functions and suffer from cognitive deficits.”
“The inflammation pathway is a key natural defense to the virus,” said co-first author Tancredi Massimo Pentimalli. “But when we block viral replication with antiviral drugs, the overzealous inflammatory response could instead become damaging.”
When the researchers treated their infected mini brains with ACV and an anti-inflammatory drug, the virus stopped replicating and the inflammation-triggering pathway was deactivated, preventing damage to the organoids.
Looking ahead: The MDC team tested two different anti-inflammatory drugs in their study and both prevented damage to the organoids. The next step, they say, is for someone to test the combination treatment in people with the deadly brain infection.
“I hope that clinical investigators will set up clinical trials evaluating the efficacy of new antiviral and anti-inflammatory combination therapies in herpes encephalitis patients, ultimately translating our findings from the bench to the bedside,” said Pentimalli.
We’d love to hear from you! If you have a comment about this article or if you have a tip for a future Freethink story, please email us at [email protected].