In the basic textbook version of genetics, DNA is the double-stranded helix that carries your genetic blueprints, and RNA is single-stranded and carries messages from DNA.
But, as always with biology, that doesn’t come close to telling the whole story.
Not only do some viruses just skip DNA altogether and use only RNA, but, in fact, RNA itself isn’t always single-stranded. Some viruses like rotavirus, scourge of children everywhere, carry their code in double-stranded RNA, or dsRNA.
Because the immune system sees dsRNA as a big, flashing virus here!! sign, dsRNA triggers the body to release protective chemicals called interferons (IFN). And that offers a unique opportunity.
Not all RNA is single-stranded. Some viruses carry their code in double-stranded RNA.
Striking a balance: Scientists are looking to harness this ability to use dsRNA as an antiviral. But the risks of this need to be balanced properly, because if the immune system kicks into overdrive, its response can become more dangerous than the pathogen itself.
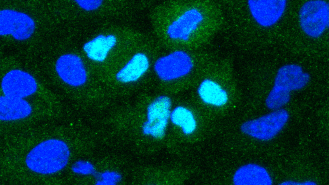
Now, researchers at the Harvard-affiliated Wyss Institute for Biologically Inspired Engineering have discovered a new class of dsRNA that gooses the right kinds of interferons (IFN-I and IFN-III), while minimizing inflammation.
When tested in human-like “organ chips” and mice, according to their paper, the dsRNA also showed the ability to combat a wide variety of viruses, including SARS-CoV-2, SARS classic, and flu.
“I’m hopeful that this RNA therapeutic technology, whose chemical and physical properties make it easily manufacturable at large scales, will become a widely used approach for fighting future pandemics,” Wyss founding director and study author Don Ingber said.
Developing the dsRNA: In earlier studies of how the immune system fights off the flu, researchers stumbled upon what they thought might be a new kind of dsRNA, which activated a new way to trigger IFNs.
To figure out exactly how it worked, the team created and tested over 200 versions of dsRNA. What they found was a specific structural quirk in the dsRNA sparked IFN production.
To gauge the dsRNA’s antiviral potential, the team — along with colleagues at the University of Maryland and NYU — pitted it against multiple pathogens in organ chips — designed to replicate the complex systems of the lung — and in mice.
Because the immune system sees dsRNA as a big, flashing “virus here!!” sign, scientists are looking to use it as an antiviral.
When the dsRNA was given to healthy organ chips, it boosted the production of IFN-I by 12-40x. When influenza A was added to the chips, the dsRNA suppressed infection by 80-90%.
After the pandemic began, the researchers challenged their antiviral candidate with coronaviruses, including the coronaviruses behind COVID-19, SARS, MERS, and the common cold.
In cell lines derived from monkeys, the dsRNA suppressed the MERS and the cold virus by over 90%, and did even better against the original SARS. When they tested it in human cell lines against SARS-CoV-2, it inhibited infection by 99.9%.
For a final test, the team turned to a mouse model for COVID-19, along with a team at the University of Tennessee. When the mice were treated with the dsRNA, they reduced viral load in their lungs by a thousand fold compared to control mice, which received just a jumbled up double-stranded RNA sequence.
“These new dsRNAs are an attractive treatment option for COVID-19 because SARS-CoV-2 infection produces an imbalanced immune response in which the protective IFN reaction is suppressed while the inflammation reaction is elevated,” Haiqing Bai, co-first author of the study, said.
“By preferentially increasing IFN-I, our dsRNA has the potential to correct this imbalance, and could be used to treat many other viral diseases as well.”
The new dsRNA was able to suppress numerous viruses.
A broad-spectrum weapon: As well as helping to fight various other viruses, the team believes that dsRNA’s immune-sparking abilities could help treat infections from other pathogens, like parasites and bacteria, and even other conditions like cancer and autoimmune diseases — basically, anything where having more of the right kind of IFN could help.
There’s work to be done before they get there, however. Figuring out the right time to introduce the dsRNA will be crucial: doing it too late could spark the very out-of-control immune response they hope to avoid.
If it all works, having a broad-spectrum antiviral therapy could be a hugely important public health tool.
“The COVID-19 pandemic has made it painfully clear that we need broad-spectrum therapeutics that are capable of attenuating infection by a wide variety of viruses,” Ingber said, “rather than developing a bespoke treatment for each individual disease as it arises.”
We’d love to hear from you! If you have a comment about this article or if you have a tip for a future Freethink story, please email us at [email protected].