A new drug delivery tech could help ensure you never miss a dose of your prescription medications — and maybe even make chemotherapy less painful for cancer patients.
The challenge: Lots of health conditions require patients to stick to a regular regimen of meds — daily or multiple times throughout the day. If you’re on multiple meds (and 24% of American adults take four or more daily prescriptions), the schedule can get complicated fast.
Not only is that a headache, it also puts patients at risk — missed doses may cause health problems to worsen, while accidentally taking too much can cause serious side effects.
“This is a huge problem in the treatment of chronic disease,” said Kevin McHugh, an assistant professor of bioengineering at Rice University. “It’s estimated that 50% of people don’t take their medications correctly.”
Existing time-release medications tend to unload their payloads unevenly.
Time-release medications can alleviate some of the burden on patients — instead of immediately releasing one day’s worth of meds, they can be packed with a week’s worth, for example, and designed to administer the drug over the course of seven days.
The challenge with existing time-release medications is that they tend to unload their payloads unevenly, with a lot of the drug being released early on in the window and very little toward the end of it.
“Most of the time it’s really problematic, either because the day-one dose brings you close to toxicity or because getting 10 times less — or even four or five times less — at later time points isn’t enough to be effective,” said McHugh.
What’s new? McHugh and his colleagues at Rice University have now designed a new time-release drug delivery tech that makes it easier to control when and where payloads are released in the body.
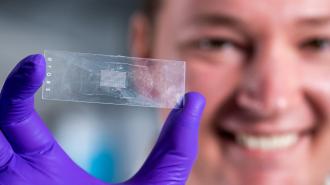
They call it PULSED (which stands for “Particles Uniformly Liquified and Sealed to Encapsulate Drugs”), and it starts with tiny cylindrical microparticles made of the polymer PLGA, which is biodegradable and biocompatible (meaning it’s not harmful to the body).
The microparticles can be filled with a drug, sealed with the application of a little heat, and then injected into a patient with a standard hypodermic needle.

By tweaking how they made the polymer, the Rice team found they could control how quickly the microparticles dissolved and released their drugs — some formulas dissolved in just 10 days, while others lasted 5 weeks.
This means a drug maker could space out when a medication is released in the body, over very long time periods, just by including a mix of microparticles that dissolve at different speeds.
While this isn’t the first time anyone has explored PLGA particles for time-release drug delivery, previous methods for sealing them were impractically expensive — the Rice team’s sealing process is fast and easy, which should help with scaling up the new drug delivery tech.
Looking ahead: The Rice team hasn’t yet determined a time limit for its new drug delivery tech, but previous research has found that PLGA microparticles can be designed to release meds as far as six months after injection, opening the door to a huge number of potential applications.
Multi-dose vaccines could instead be delivered with a single injection; with the right mix of their microparticles, your “second dose” could dissolve right on cue, weeks or months later — without another trip to the doctor.
Researcher Tyler Graf also believes it could possibly improve the treatment for the most common cause of severe vision loss in seniors, wet age-related macular degeneration (AMD), which typically involves a series of injections directly into a patient’s eye.
“One application we want to do is inject different populations of these microparticles into the eye so that we can mimic clinical dosing schedules,” said Graf, “so that instead of getting an injection every month, we can space that out to an injection every three months or six months.”

The new drug delivery tech might even be able to improve cancer treatment. For their study, the team made the microparticles in a variety of sizes, and if doctors loaded the largest particles with chemo and then injected them at the site of a tumor, they could deliver targeted treatment.
“Our microparticles will stay where you put them,” said McHugh. “The idea is to make chemotherapy more effective and reduce its side effects by delivering a prolonged, concentrated dose of the drugs exactly where they’re needed.”
We’d love to hear from you! If you have a comment about this article or if you have a tip for a future Freethink story, please email us at [email protected].