Seeing the world’s most advanced bionic arm in action is kind of mind blowing. Johnny Matheny, the man who wears it, lost his left arm to cancer eight years ago. Thanks to the Applied Physics Laboratory at Johns Hopkins University, he basically has a left hand again.
If you haven’t watched the episode, go do that! And then read our interview–edited for length and clarity–with Michael P. McLoughlin, the chief engineer of research and exploratory development at the APL. It’s basically a one-stop guide to the present and future of bionics.
Let’s start with this: How does Johnny’s arm work?
If I have an amputation and I think about moving my hand or wiggling my fingers, the brain produces those signals and they travel down the nerves, but once they hit the amputation, they have no place to go because the hand is gone.
So what you can do is take the nerve that, say, used to run to finger and can attach that to a different piece of muscle. So now when I think, “Move my finger,” a different piece of muscle somewhere in my arm or chest will contract and I can measure that contraction. This surgical procedure is called targeted muscle reinnervation.
For somebody that’s operating the prosthetic as an amputee, they get this procedure and then when they think, “Move my finger,” a little piece of muscle in the chest vibrates, and the arm knows that if that piece of muscle vibrates or moves, then that means it needs to move the prosthetic finger. In effect, it’s a way that we can communicate with the brain without actually having to implant something in the brain. For an amputee, who has an intact peripheral nerve system–those are the nerves that leave the brain–targeted muscle reinnervation turns out to be a very, very straight-forward way for them to control a prosthetic limb.
What’s the learning curve for using targeted muscle reinnervation with a bionic prosthesis?
Intuitive control is really important. Think about what you do with your hand, the way you move your fingers. Now suppose I let you control a prosthetic limb or bionic arm and give you an Xbox controller with a little joystick on it and a few buttons, and I tell you, “Make the arm do this, okay?” It’s very difficult for you to take that thought–which we do very naturally and with very little concentration–and convert that into “How do I move the joystick?” and “Which buttons do I push?”
It would take even an experienced gamer days, if not weeks or months, to get really any level of proficiency at that. But you and I do it all the time. We move our hands and we hold objects and we hardly give it a thought. So that’s what we want to really be able to do, is translate that thought, that intuitive thought, into actions of the prosthetic without having to go through these intermediary, unnatural types of things.

And I think that’s why many of the people who have used the modular prosthetic limb say they don’t really consider it as a machine. They really feel like it’s an extension of themselves because the brain thinks, “Move my hand,” and the hand moves in a way they would expect it to move, so it’s a very natural thing.
So reinnervation combined with the prosthesis means amputees can do things. Can they feel things?
Targeted muscle reinnervation reconnects some of the nerves that bring sensation, say from the finger back to the brain. So now if I press wherever that nerve happens to be, the brain interprets that as, “Hey, I’m getting a signal from my finger.” The amputee will actually say, “I feel my finger again.” It’s not, “I feel something on my arm or chest,” it’s “I feel my finger.”
Right now, the modular prosthetic limb has over 200 sensors in it, and we’ve just used a small fraction of those. What we really see in the future, as we get better at this and we get better connections to the brain, is being able to provide a much greater wealth of signals back.

I always compare it to the Internet because everybody understands the Internet, right? Back when nobody knew about the internet, it was a big deal to send a text message. Today, we get frustrated if we have trouble downloading an HD movie. With this technology, we’re still sending text messages; we have very low information channels to the brain. We’re still able to do remarkable things with those channels, but just think what happens when we start scaling this and it goes up by a factor of ten–a hundred, a hundred thousand–what we’ll be able to do.
What other kinds of disabilities can this technology address? It can’t just be amputees, right?
So we’ve started this program for amputees and people with spinal cord injuries, but if you think about it, what are all the other types of disabilities that people have? Stroke, ALS. These people have trouble getting around, they lose their eyesight. These are all things that are due to the fact that our bodies sometimes can’t do what our brain commands.
I’m getting a little older now. I can still think about doing all the things that I did when I was 20 years old, but my body can no longer do them. This technology is opening up a channel that helps us assist the body in doing those things. So as we lose our mobility, as we lose our strength, as we lose our eyesight, as we lose our hearing, we can actually begin to replace that.
(A)s we lose our mobility, as we lose our strength, as we lose our eyesight, as we lose our hearing, we can actually begin to replace that.
There are some remarkable things already. We have people with Cochlear implants who are able to hear again. There are retinal prosthesis for blindness that have some of level of success. Those are still very early, but I think the promise of all this is that we’re beginning to reach back into the brain. Right now we give people artificial knees and artificial hips. Soon we’ll be able to give them so much more.
Why did you start with a bionic arm?
We focused on arms because the arms are very complex, and if you think about all the things you do–eating and fixing meals–you need them. We’ve solved the mobility problem with wheelchairs and other devices pretty readily. But for somebody who doesn’t have use of their arms anymore, there’s really not much out there for them. That’s where this advanced bionic arm comes in.
Can you talk about some of the challenges of rebuilding one of the more complicated body parts and connecting it to the brain?
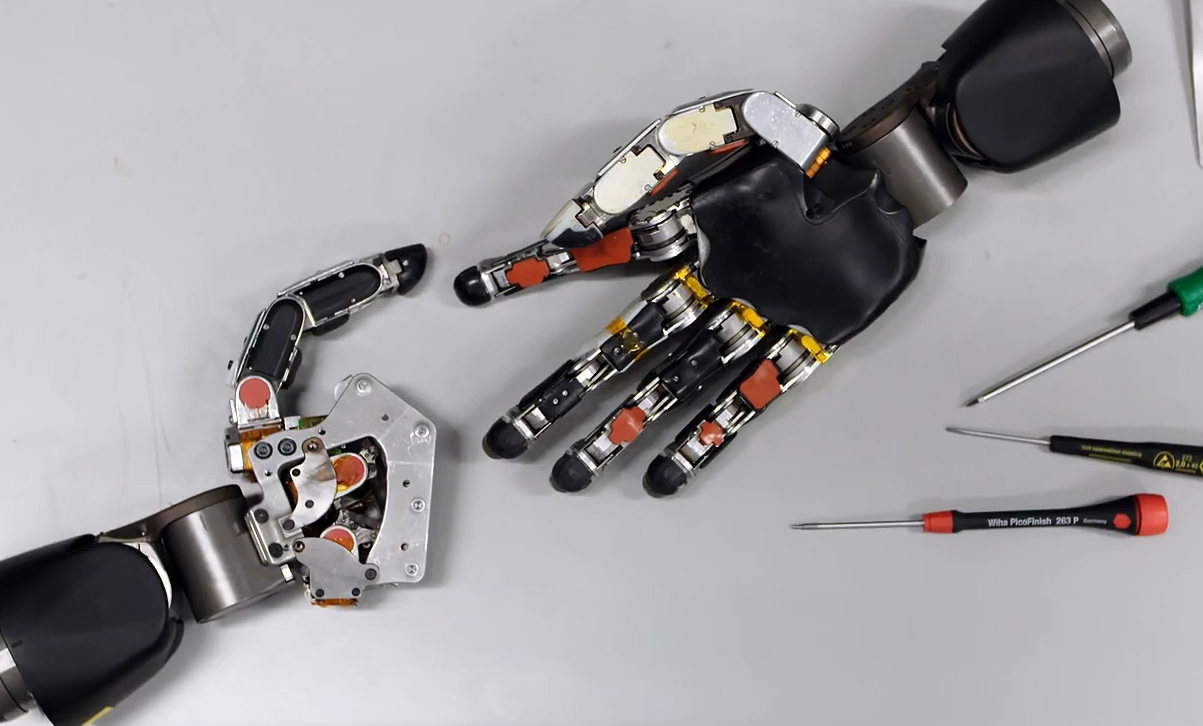
There are two major challenges. The first one was being able to determine the brain’s intent: what did you want to do, how did you want to move your arm, how did you want to position your hand. The second thing was making a device that could actually replicate what we do with a hand. So you think about all the individual joints and being able to move fingers individually. It’s a very complex system. It’s also complicated when you think about size versus strength: We can curl 40, 50 pounds, we can pick up a jug of milk. To be able to replicate all that in a device that still looks like a human arm and weighs about the same as a human arm is a really difficult engineering challenge.
So this is basically a huge step up from the status quo of upper extremity prosthetics.
When you think about what’s happened in lower extremity prosthetics, we’re arguing about whether somebody with an amputation should run in professional sports because their prosthesis might give them an unfair advantage. You’ve never heard anybody make that argument about an upper extremity amputee. So the challenge to us was, how do we get somebody from the level of wearing a hook to a level where they can do the types of things that they did with their natural limb?
(H)ow do we get somebody from the level of wearing a hook to a level where they can do the types of things that they did with their natural limb?
We want to have that same argument about upper extremity prosthetics. For people to say, “It’s not fair because they have a prosthetic.” We’re not there yet, but a lot of the fundamental technology is there. And one of the challenges that we have is that it’s a much smaller population and so it doesn’t have the business drive that brings people into lower extremities research, or to fight diseases like diabetes that have much bigger populations (ed note: diabetes can lead to neuropathy in the lower extremities, which often leads to amputation).
Spinal cord injury seems different than amputation. Can you talk about prostheses for people who aren’t missing limbs, but rather have a damaged nerve pathway?
For somebody that has a, say, a spinal cord injury, they’re still able to think about moving their arm, but now for some reason–either because of a physical injury or a disease–the signal can’t get from the brain to the body. Those nerves all still light up and they make little electrical signals, those signals just have nowhere to go. The signal is trapped.
As an electrical engineer, I think of that as a broken cable somewhere. So what we can do in that case is actually insert very small electrodes into the area of the brain that, say, controls the arm. By doing that, we’re now able to actually measure those signals. And by using computer algorithms, we can then look at essentially the codes of the brain and interpret that set of patterns. This one means I’m going to reach out in a certain direction, or that I’m going to open and close my hand, or that I’m going to shake my fingers in a certain way. And basically we just bridge that gap. It’s very similar to what we do in some of the cases with amputees, but in the spinal injury case, we go directly to the brain.
What we want to give that person who has a spinal cord injury is the ability to naturally move an arm. It doesn’t matter if the arm is right next to that person and she wants to eat a chocolate bar, or if it’s on the other side of the room and she wants to prepare a meal.
What we want to give that person who has a spinal cord injury is the ability to naturally move an arm. It doesn’t matter if the arm is right next to that person and she wants to eat a chocolate bar, or if it’s on the other side of the room and she wants to prepare a meal. What it does is give her the chance to move beyond her physical limitations and begin to interact in the world again in a way that she couldn’t. And if you ask many of these patients what they’re thinking about when they used the technology, they just say, “I’m thinking about moving my arm.” It’s not a mechanical device, it’s an extension of themselves.
There’s a really compelling psychological component here that transcends the technology.
Our goal in this whole project is to give back something that was lost. The ability to reach out and pick up food so that we can feed ourselves or reach out and touch another individual is just a huge thing for all of us. Just imagine if you can’t do that anymore, if you can interact with somebody, talk to them, but you can’t physically interact with them unless they reach out and touch you. When all of a sudden that starts to come back and you give somebody the ability to move a limb, or replace a limb that’s lost, it’s an intensely powerful experience.

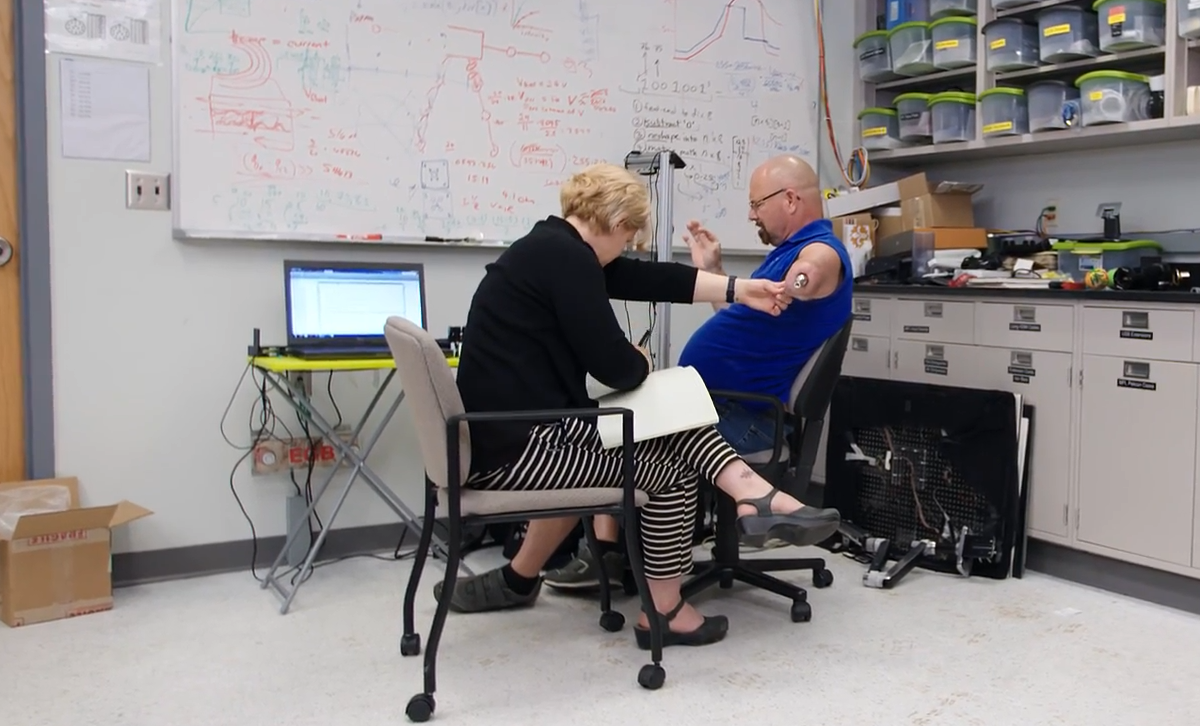
Frequently we’ll have somebody that is an amputee say, “Hey, I’m thinking about maybe having targeted muscle reinnervation surgery, and I’d like to just come in and try the arm out and see what it’s like.” So what we can do is we can actually put electrodes on whatever residual arm limb that they have. We’ve seen in several instances where we hook up the electrodes and say, “Okay, think about bending your elbow,” and in a few seconds, they’re bending the elbow. And I’ve literally seen people burst into tears. It’s like, “Oh my God, I haven’t been able to do that in 5, 10, 20 years.” And it’s just incredibly powerful. That simple thing–just bending their elbow–has just a tremendous impact on them. So you just imagine the possibility when we give them the ability to actually do what I’m doing now, what that’s going to mean to them.
The arm doesn’t look like a human arm, though. It looks very much like a robot arm.
When we started this program, we thought a lot about the need to make cosmetic coverings so that if I looked at the prosthetic, it actually looked like my real hand. But what we found is that wasn’t really the important thing. What was really the important thing was that it moved and functioned like the hand that was lost.
As a matter of fact, a lot of the younger military personnel we worked with felt having a black robotic arm is kind of like a cool thing. They don’t want it to look like a natural arm. But overwhelmingly, it’s that functionality that matters–that it’s an arm and not some mechanical device that’s moving around. People want the fluidity and the range of motion and everything that they lost. When you give that back, it’s just a tremendous experience. The patients we’ve been able to work with are just a remarkable group of men and women of all ages and backgrounds.

You mentioned that the development of upper extremity prosthetics is constrained by the small number of patients. Is that constraint changing at all?
What’s really exciting right now is that we’ve reached a point–I’ll call it a tipping point–where we’ve developed all the basic capabilities. If you were going to try to do this 10 years ago, you would’ve had to figure out how to build an arm, how to interface with the brain, and then all the algorithms to interpret that information. But today we’ve got all that, and it enables us to democratize the technology. We’ve intentionally kept the the modular prosthetic limb as an open device so anybody can interface with it. For instance, we have a prosthetic limb, and you can build an app for it. You can use that prosthetic limb for anything you want to use it for. So it doesn’t have to be for somebody, say, that has spinal cord injury. If you wanted to use it in a factory to do something, you could potentially use it for that. We’re really only limited by people’s imaginations and ability to plug into this great technology.
What’s the next step? When does this technology become a normal part of daily life for amputees and people with disabilities?
With the technologies that are ready to go today, it’s primarily an investment problem. When we talk about amputees, it’s a fairly small population of patients. A very complex robot device that can mimic the human hand costs hundreds of thousands of dollars. In order to develop the volume and get the cost down, you need to have multiple applications that go beyond just the prosthetic space. That market just hasn’t developed yet. There’s a lot of interest in it, but we really need to develop applications where we can take this technology and use it for other things that will eventually drive the cost down. So we really need a combination of further advancement in the technologies, but also investment and business expertise to help move this forward.
The thing that keeps myself going and Albert Chi going is that we’re reaching the point where this can really break out and get into the home and stay with people in their everyday lives. That’s the threshold that we want cross now.






