In many countries, many people with mental illnesses go undiagnosed, meaning mental health is given less attention and support than it deserves. Even for those diagnosed, treatment can be of poor quality, if they receive it at all.1
To reduce the burden of mental illnesses, the world needs reliable data, which includes the number of people that face mental illnesses, how and when they occur, and the effectiveness of treatments.
How are mental illnesses defined?
Defining mental illnesses is complex. They are diagnosed based on people’s psychological symptoms and behavior rather than biomarkers, brain scans, or blood tests. This makes them more subjective – they are dependent on whether people share their symptoms and the way doctors diagnose them.
Mental illnesses are formally defined according to the International Classification of Diseases (ICD) and the Diagnostic and Statistical Manual of Mental Disorders (DSM). The ICD is used internationally by healthcare professionals, while the DSM is primarily used by psychiatrists in the United States.2
These manuals explain how to diagnose mental illnesses by observing and asking about people’s symptoms and behavior, and the context of their symptoms – for example, symptoms that appeared because of drug use or other medical conditions don’t qualify as mental illnesses.
Based on these definitions, healthcare professionals can make diagnoses, which can be used for healthcare, treatment, and national statistics.
Over time, the definitions of particular mental illnesses have changed. The DSM has been revised 5 times since it was first developed in 1952, while the ICD has been revised 11 times since 1900.3 They will continue to be revised in the future, but updates have become less frequent.
Their changes are partly due to a better understanding and measurement of mental illnesses. They have also changed as a result of cultural and legal factors. There used to be larger differences in the criteria for diagnosing mental illnesses between the ICD and the DSM, but the two manuals are now more similar due to collaboration between their developers.4
Mental health data based on diagnoses
The process of diagnosing a mental illness usually starts with the patient consulting a healthcare professional.5 This can be a doctor in a clinic or general hospital, a psychiatrist, or another mental health specialist.
Health professionals use official medical guidance and professional judgment to decide whether to diagnose a patient with a condition.
Data on these diagnoses are collected from hospitals in many countries, but this may not include clinic visits. The data can include people’s age and sex, their reason for admission, other diagnoses, and treatments given during their visit.6
What are the strengths and limitations of diagnosis data?
Strengths of data based on diagnosis
Official data from diagnoses of mental illnesses have two major strengths.
First, the diagnoses come from healthcare professionals with training and experience in recognizing mental illnesses.
They can use their knowledge to ask people more questions about their symptoms and understand their context before making a diagnosis. They can also perform additional medical tests to rule out other conditions.
Second, data on diagnoses can tell us about the number of people who seek out mental health treatment from public hospitals and clinics. This can usually be linked to data on which treatments they were prescribed and for how long.7
This can be very useful for countries to understand the resources used to treat mental illnesses.
Limitations of data based on diagnosis
Data on diagnoses of mental illnesses also has limitations.
One problem is that many people do not reach out to healthcare professionals about their health conditions. This might be because they lack awareness of mental illnesses or there is a lack of healthcare for these conditions in their country. They may also feel uncomfortable about sharing their symptoms with healthcare professionals.
Another problem is that the diagnoses may not be made consistently. Doctors can have different levels of training and experience in recognizing and diagnosing mental illnesses. This can be a problem when comparing diagnosis rates between countries.
A third problem is that national data on diagnosis is often collected from a limited number of sources. Data from private hospitals and clinics is usually not included. In some countries, mental health data is collected from hospitals but not clinics.8
Some countries also use data from other sources. For example, the data might come from health insurance claims—which include private healthcare—or from other databases connected to many healthcare clinics across the country.
The final problem is that countries may use different definitions to diagnose patients. Some countries use modified versions of the ICD manual to collect their data, depending on their cultural context and needs.9
These differences mean that comparing data between countries using data on diagnoses can be difficult.
Mental health data based on surveys
Aside from the formal diagnoses, mental illnesses can be measured using surveys and screening questionnaires.
These tend to ask people about symptoms similar to those in diagnostic manuals, but they can be used more easily and widely because the data does not need to be collected by a healthcare professional.
These surveys can be conducted in different ways: over the phone, online, or in-person while anonymized.10
During the surveys, trained professionals ask people in the general population whether they have experienced symptoms of mental illnesses. They also ask about the age when people first experienced them, how long they lasted, and how severe the symptoms were.
People may be asked about symptoms they have currently, or have had recently, or in their lifetime so far.
Some symptoms of mental illnesses may be common in the population. This chart shows data from a US survey called the National Health and Nutrition Examination Survey. It was a large-scale, in-person survey of people in the general population.11
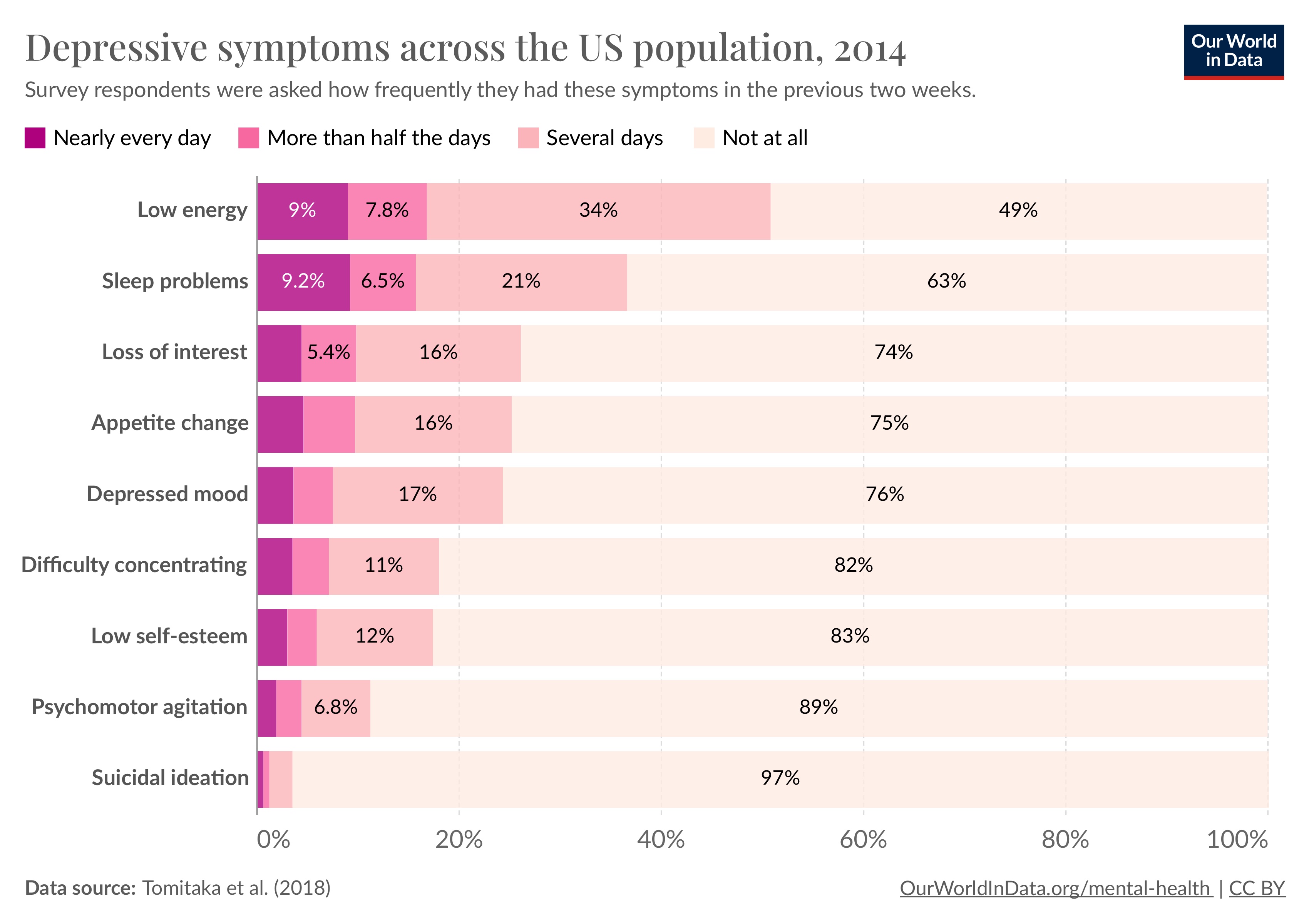
As you can see, around a fifth of the US population says they have had a depressed mood for several days in the past two weeks.
But having one or a few symptoms does not necessarily mean that someone can be diagnosed with depression. Instead, researchers look at the combination of symptoms that people report. They will set a threshold for the number of symptoms someone must have before they are considered to have the condition.
To diagnose someone with major depression, for example, the ICD and DSM criteria require them to have had a depressed mood or loss of interest for much of the day, nearly every day, for at least two weeks, along with several other symptoms.
What are the strengths and limitations of survey data?
Strengths of survey data
Survey data on mental health has two major strengths.
First, it involves structured interviews – people are asked a consistent set of questions regardless of their interviewer. This helps to ensure the data is more comparable between interviewers and across time.12
Second, surveys include a much wider range of people in the population, including those who would not seek treatment due to a lack of awareness, costs, or other concerns.
This can help to understand the prevalence of mental illnesses in the general population, including people never diagnosed by a healthcare professional. This can help us understand what share of people seek treatment.
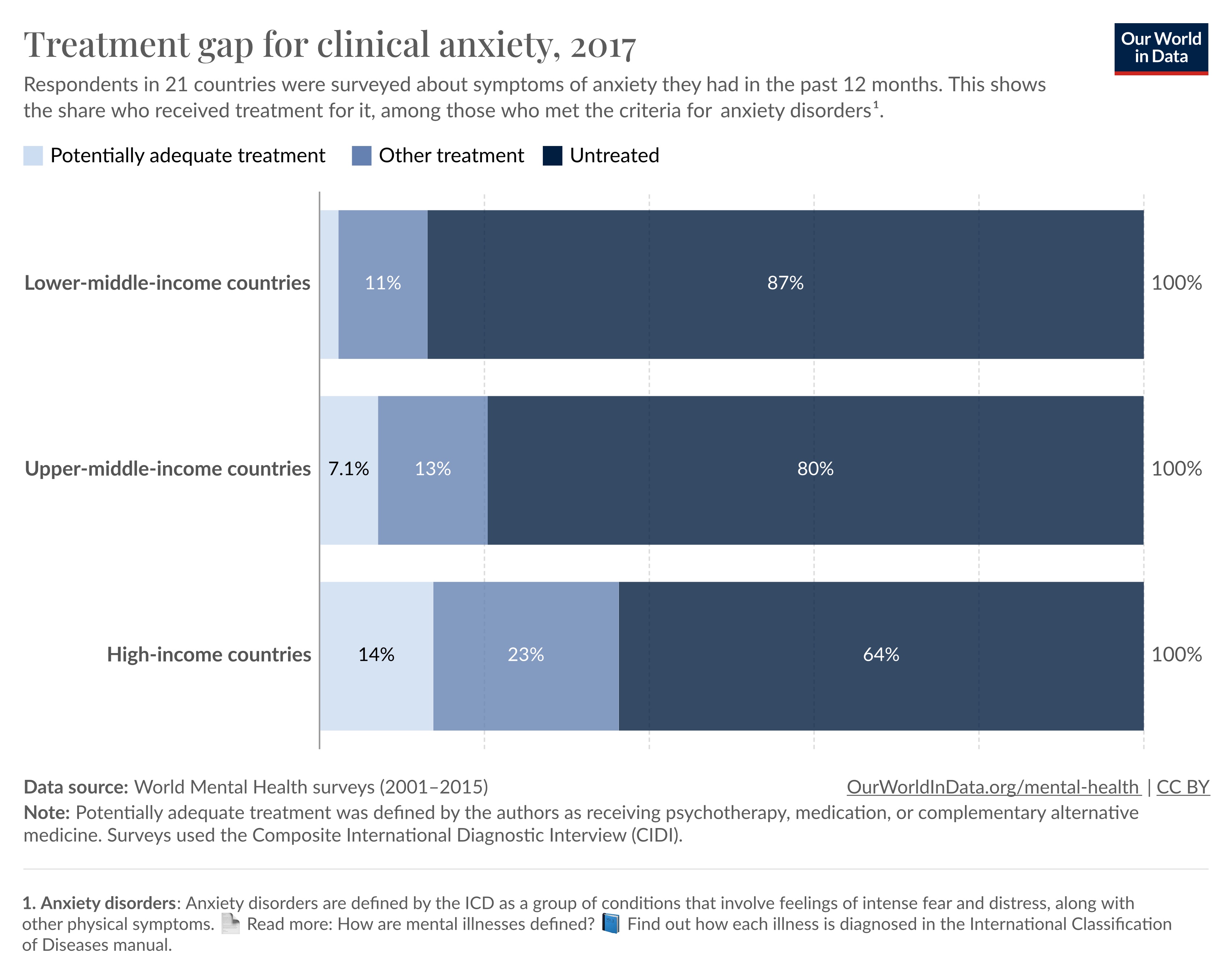
One example is the World Mental Health surveys: these were large-scale surveys of mental illnesses in the general population in 21 countries of different income levels.13
Based on structured interviews, the authors found that around 1 in 10 people met the criteria for an anxiety disorder in the past year across countries surveyed.14
In the chart, you can see the share of those who met the criteria who also said they had received treatment. Only around 36% with anxiety disorders received any treatment in high-income countries, while an even lower share – only 13% – received it in lower-middle-income countries.15
Third, surveys can tell us about milder symptoms that may be common in the population. This can help to see if a condition lies on a spectrum – where everyone has the symptoms to different degrees – or if it affects a separate share of people.
Limitations of survey data
There are also several limitations of survey data to keep in mind.
One is that people may not share their symptoms in surveys, as they may not feel comfortable sharing them with researchers. Along with this, people’s comfort in sharing mental health symptoms may vary between countries and over time.16
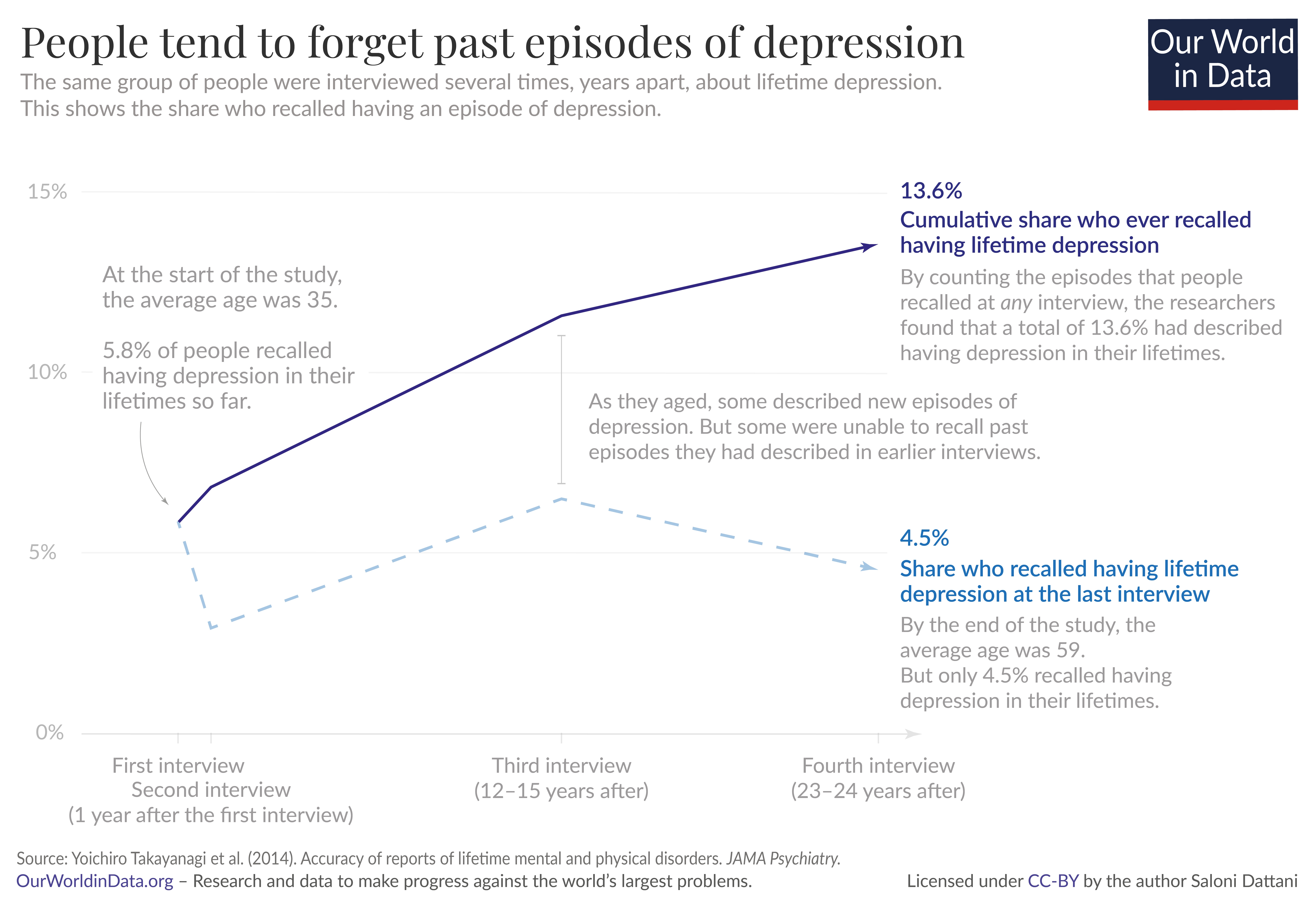
Another limitation is that people may not remember their symptoms, especially when they are asked to recall symptoms in their lifetime so far. This can be challenging for older people whose symptoms may have occurred decades ago.
This chart shows data from a study where the same people were interviewed several times about depression in their lifetimes so far.17Around two-thirds of people who had described episodes of depression did not recall them in subsequent interviews.
A third limitation is that survey data does not usually exclude other diagnoses. When people visit a doctor for a diagnosis, the doctor may ask them about other existing conditions and medications they are taking, and test them for other medical conditions which could also cause their symptoms. This is not usually performed in surveys.
It can also be difficult to compare people’s responses in surveys, because people may interpret the questions differently. This can make it difficult to compare people from different backgrounds, languages, and countries.18
Another consideration is who is included in surveys. Some include people from a wide range of backgrounds in the general population, while others only include particular groups like urban residents or university students.
This can be a big problem for mental health conditions that are less common, such as schizophrenia and bipolar disorder. If only a few people in the study had a condition, then it can be difficult to estimate the precise share of the total population with it.
It’s also important to know that surveys of the general population usually do not include people who are institutionalized in hospitals or prisons, who may have more severe physical and mental health conditions.19
How much data on mental health is available around the world?
Data on mental health varies in two ways: the amount of data on each mental illness and the amount of data from each country.
First, there is much more data available on some mental illnesses than others.
You can see this in the chart. It shows the number of countries with primary data on the prevalence of each mental illness in the general population. The studies were used by the IHME’s Global Burden of Disease study to estimate the prevalence of mental illnesses worldwide.20
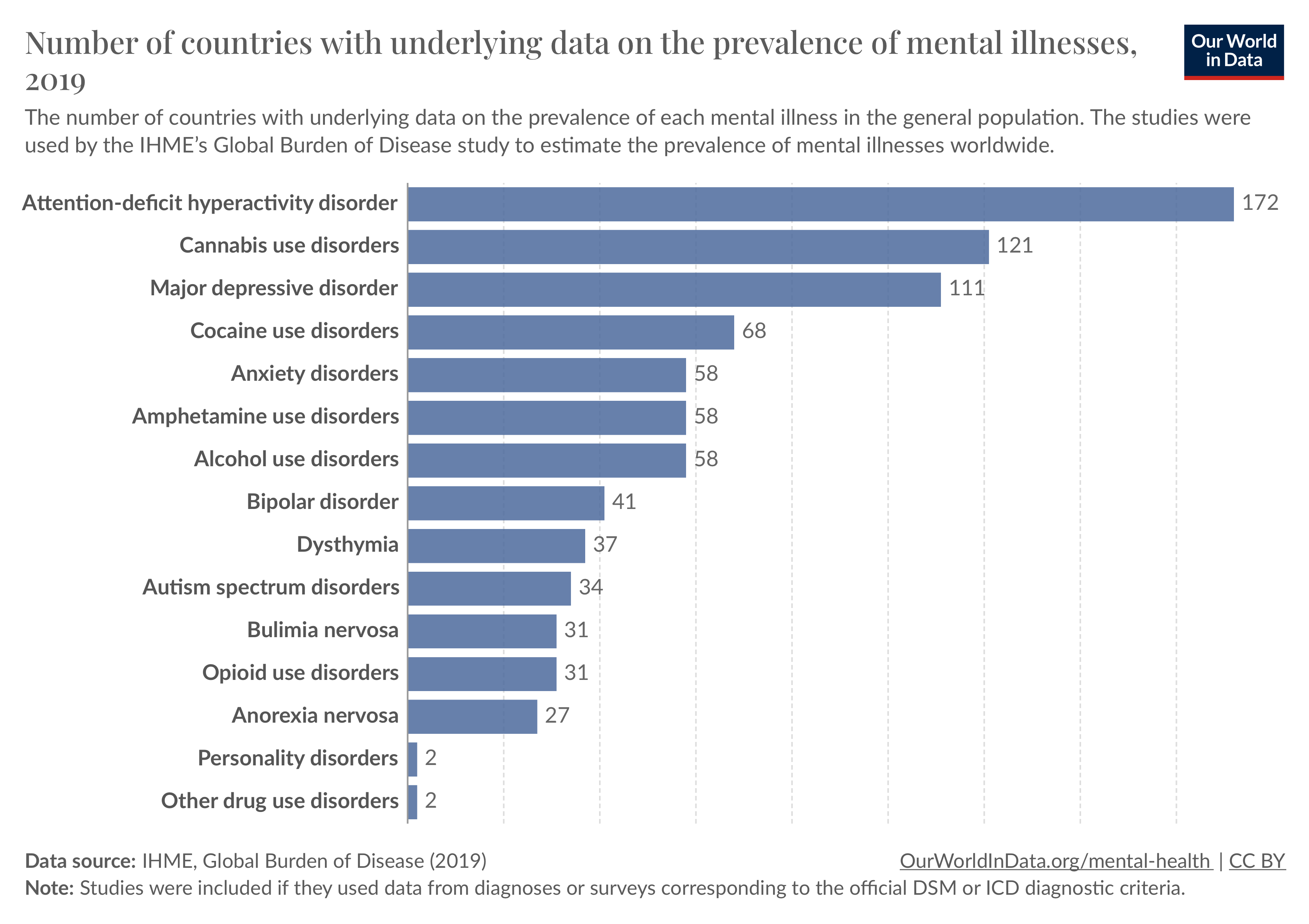
As you can see, data on some mental illnesses such as attention-deficit hyperactivity disorder, cannabis use disorder, and major depressive disorder came from a large number of countries.
However, data on others, such as bipolar disorder, autism spectrum disorders, and anorexia nervosa, came from fewer than 40 countries. For personality disorders, data came from only two countries.
Second, there is much more data available from some world regions than others.
In this chart, you can see the share of the population of world regions that had any data collected on the prevalence of major depression between 1980 and 2008.
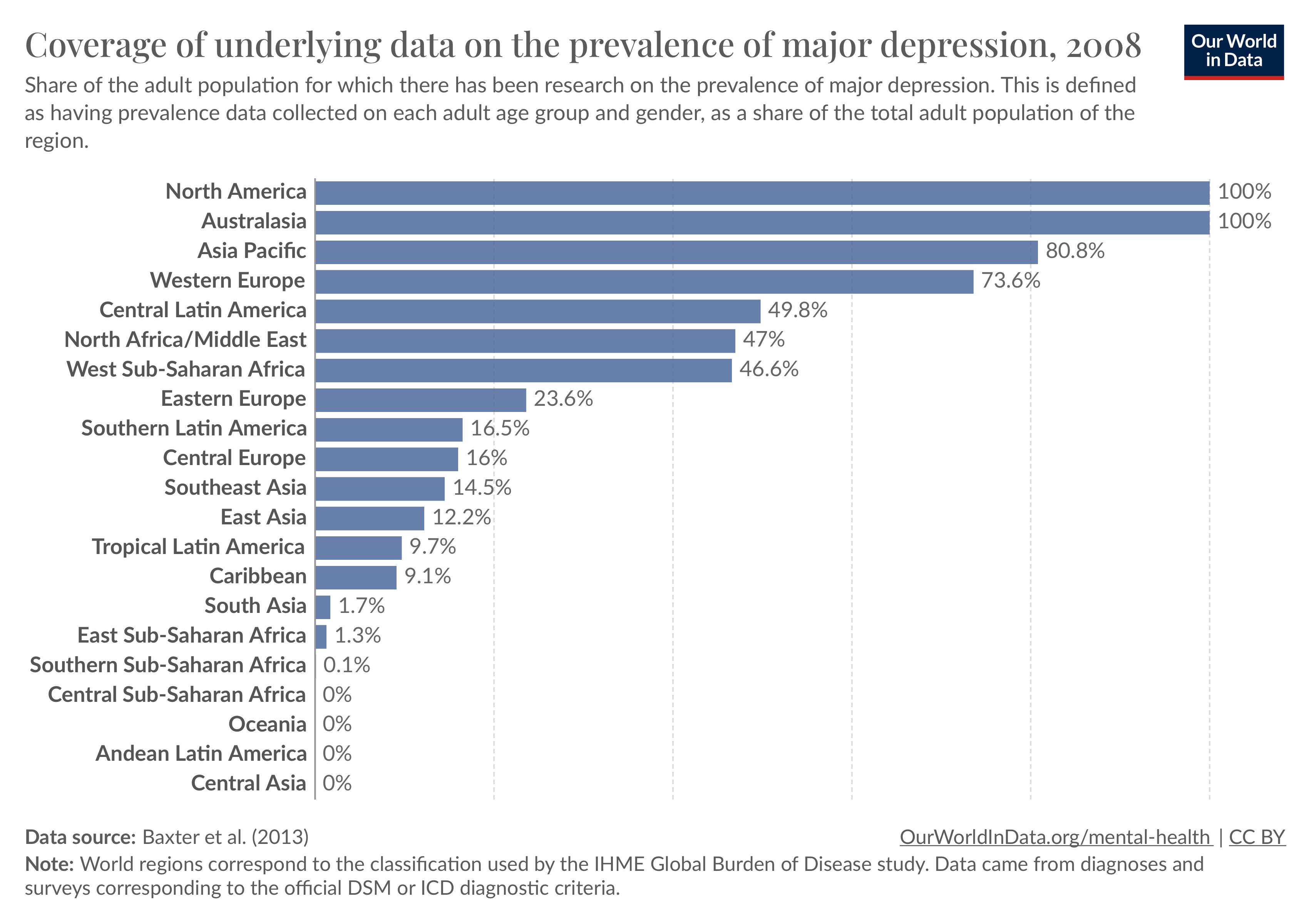
This comes from an older study published in 2013, and more data has been collected since then, which has helped improve estimates made by the Global Burden of Disease study.21
In Australasia and North America, there was data relating to all of the age demographics in the population. But in regions such as Eastern Europe and Southeast Asia, less than 25% of the population was covered.
In several regions, especially in sub-Saharan Africa, Central Asia, and South America, there was almost no underlying data available.
What about other mental illnesses apart from depression?
In the chart, you can see the population that was covered in data on other common mental illnesses.
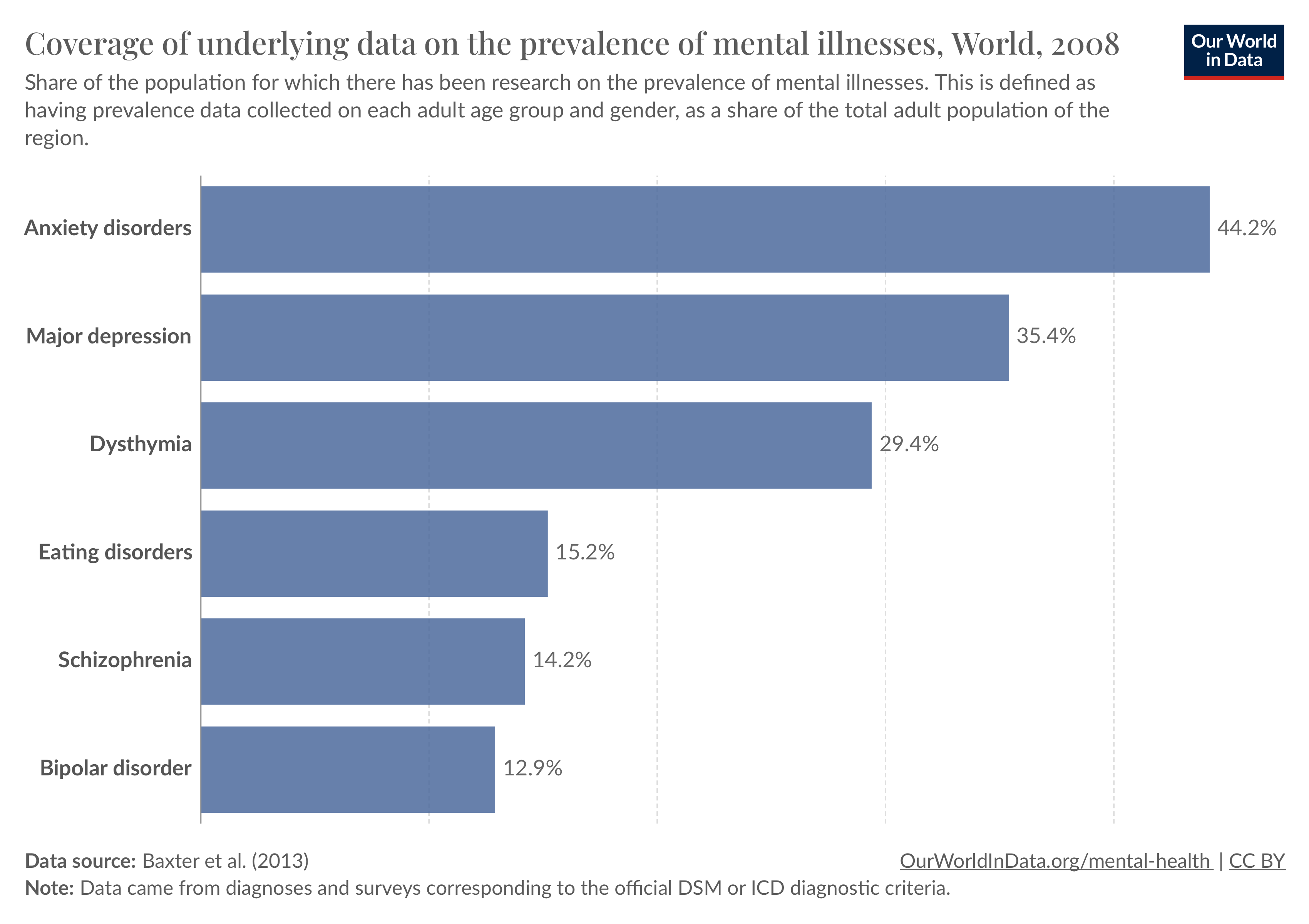
As you can see, there was more data available on anxiety disorders and major depression than on schizophrenia and bipolar disorder.
How do researchers extrapolate this data to make comparable estimates?
Researchers can try to make comparable estimates of mental health using this underlying data and statistical methods.22
These methods incorporate the available data on people’s mental health, their demographics, and the level of diagnosis and testing. Then they extrapolate the results to other countries, where data has not been collected. This can be based on demographics such as age and sex, other risk factors, responses to other large-scale representative mental health surveys.23
They try to adjust for the fact that the underlying data was collected from different sources (diagnoses or surveys), during different periods, and from different groups of people.
However, they come with a range of uncertainty. This is because they rely on assumptions about how the data was collected, and why some demographics and countries lacked data on the prevalence of mental illnesses.
This is especially true for some illnesses – such as eating disorders and bipolar disorder – and some world regions – including much of Asia, South America and Africa; where primary data is lacking.
Data on global mental health is limited – but nevertheless gives us important insights
Data on global mental health has two main limitations.
First, our understanding of global mental health depends on people’s willingness to share their symptoms, and contact healthcare professionals to receive a diagnosis and treatment. Because of this, many people remain undiagnosed and lack support and treatment.
Another major limitation is that data is lacking in many countries. It is often available only for some age groups, and is collected by separate one-off studies at infrequent intervals. There is much less data available for some illnesses than others.
For countries that lack data, the prevalence of mental illnesses is estimated from other similar countries with data, but this leads to large uncertainties.
Despite these limitations, the available data does give us important insights:
Importantly it shows that mental illnesses are not uncommon. For example, the World Mental Health surveys estimated that one-in-ten people met the criteria for anxiety disorders in the past year, on average, across countries.24
Global data also tells us that mental illnesses have a large treatment gap, especially in poorer countries. For example, while around one-in-three with anxiety disorders received any treatment in high-income countries, less than one-in-eight did in lower-middle-income countries.
Mental illnesses are a major part of the global health burden and remain untreated for many people. To address this, countries need more data on these conditions for a wide range of demographics, and long-term data to understand how they develop, and how effective the treatments are.
Republished with permission of Our World In Data under a Creative Commons license. Read the original article.






