Japanese researchers have discovered a way to improve a walking condition known as “Parkinsonian gait” by painlessly zapping patients’ brains every time they take a step.
The challenge: An estimated 8.5 million people worldwide live with Parkinson’s, a progressive neurological disorder that often leads to problems with movement, including stiffness, tremors, and a distinct walking pattern known as “Parkinsonian gait.”
Deep brain stimulation and medications for Parkinson’s aren’t as effective at addressing gait disturbances.
People who develop Parkinsonian gait typically take small, shuffling steps and may have trouble starting walking (an issue known as “freezing of gait”). Symptoms are often worse on one side of the body, and because they can have trouble picking up their feet, people with Parkinsonian gait are at increased risk of falling and injuring themselves.
While deep brain stimulation and some medications can help treat stiffness and tremors in Parkinson’s, they aren’t as effective at addressing gait disturbances. Additionally, deep brain stimulation requires invasive surgery, while the drugs can cause unwanted side effects.
What’s new? Researchers in Japan have now demonstrated how a non-invasive brain stimulation called “transcranial electrical stimulation” (TES) can alleviate Parkinson’s gait.
“We successfully developed a new non-pharmacological and non-invasive intervention for the rehabilitation of patients with [Parkinson’s] and other neurological disorders,” said senior author Yoshino Ueki from Nagoya City University. “Our breakthrough method could be used to restore gait in these patients.”
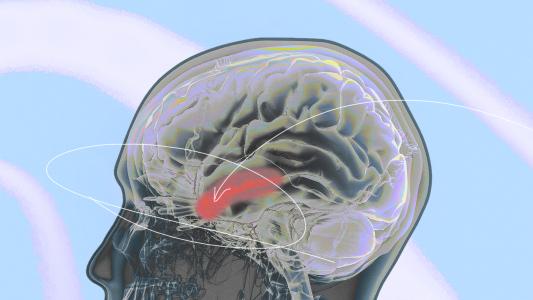
How it works: TES is a kind of brain stimulation in which an electric current is sent between two or more electrodes on a person’s scalp.
To treat Parkinsonian gait, the researchers place the electrodes around the skull so that a low current stimulates the cerebellum — a part of the brain that plays a key role in walking and movement — on the side of the body with more severe symptoms.
“Our breakthrough method could be used to restore gait in these patients.”
Yoshino Ueki
The trial recruited 23 people with Parkinsonian gait. All were over the age of 40, able to walk for at least 6 minutes on their own, and capable of performing daily tasks independently.
Using a pressure sensor placed on the floor of a corridor, the researchers got baseline walking measurements for the participants, who also completed surveys to determine the severity of their freezing of gait. Each person was then assigned to either the treatment or sham group.
Twice a week for five weeks, the participants walked down the corridor at their own pace for 16 total minutes. The treatment group received brain stimulation that was timed to coordinate with each step of the foot on their “bad” side. The control group received a sham stimulation expected to have no therapeutic effect.
By the end of the study, walking speed, step length, and gait symmetry had significantly increased for people in the treatment group, but not those who received the sham stimulation. Treated participants also reported less severe freezing of gait than at the start of the study.
Looking ahead: The study had several limitations, including its small size and the fact that some participants were on medications that could have affected their results.
Still, the results suggest that TES deserves a closer look as a potential treatment for Parkinsonian gait. Future studies could test different levels or patterns of stimulation, explore the durability of the therapy, and test whether it can help people who are more severely affected.
“Our novel intervention might be able to improve physical function for not just patients with [Parkinson’s] but also for those with other disabilities,” said Ueki.
We’d love to hear from you! If you have a comment about this article or if you have a tip for a future Freethink story, please email us at [email protected].