By creating a “bridge” between chemo drugs and cancer cells, Australian researchers may have solved the problem of effectively treating kids with high-risk leukemia without subjecting them to severe side effects or lifelong health issues.
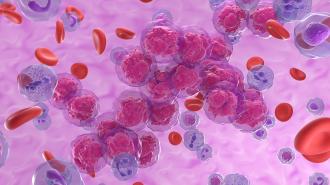
The challenge: Leukemia is a type of cancer that starts in the blood cells and bone marrow. It’s the most common cancer in children, but thankfully, it’s also highly treatable — 90% of kids with the most common form of the disease remain in remission five or more years after treatment.
Getting rid of the cancer is much harder for kids with “high-risk” leukemia, though. These cancers have already proven difficult to treat, or have characteristics that make them resistant to treatment, such as certain proteins on the surface of the cancer cells.
Doctors have to take a more aggressive approach to treat patients with high-risk leukemia, administering higher doses of chemo. This not only increases severe side effects, but also raises the risk of lifelong health issues due to the drugs’ collateral damage on healthy cells.
“By specifically targeting leukemia cells, we can make treatment more effective, as well as much safer to use in children.”
Maria Kavallaris
What’s new? Past research has shown that encapsulating chemo drugs in tiny particles of fat called “liposomes” can make the treatment more tolerable, but large doses are still needed, and they still tend to accumulate in healthy organs, where they cause systemic damage.
Now, researchers from UNSW Sydney and the Children’s Cancer Institute have developed a way to guide encapsulated chemo meds directly to cancer cells — and based on lab and mouse tests, it seems to work.
“Finding a way to make treatment drugs act more selectively on cancer cells is the key to improving treatment success while reducing toxicity in children treated for high-risk leukemia,” said lead researcher Maria Kavallaris. “By specifically targeting leukemia cells, we can make treatment more effective, as well as much safer to use in children.”
How it works: The hunt for a better leukemia treatment led the Aussie researchers to a type of artificial protein, called a “‘bispecific antibody,” that can be designed to bind to two different molecules, forming a bridge between them.
“We can target the same drug to any child’s blood cancer.”
Ernest Moles
For their study, they created a bispecific antibody that binds on one side to doxorubicin, a liposome-encapsulated cancer drug, and on the other side to proteins on the surface of leukemia cells. The idea is that this would ensure the chemo connects with cancer cells and tends to leave healthy cells alone.
When the researchers compared their combination leukemia treatment to doxorubicin alone in lab tests, they found that their formulation killed more cancer cells.
In mouse models of leukemia, adding the bispecific antibodies reduced the amount of the chemo drug that accumulated in the animals’ hearts and kidneys, and some of the mice treated with the antibodies lived up to four times longer than ones that received only doxorubicin.
“There will be no easy escape.”
Ernest Moles
Looking ahead: The researchers are now focused on getting their system ready for clinical trials. If it works as hoped, it could give doctors a straightforward way to tailor a leukemia treatment to each patient’s cancer.
“Rather than having to design a completely new therapeutic each time, all we need [to] do is change the antibody bridge, and we can target the same drug to any child’s blood cancer,” said first author Ernest Moles.
The approach could also help doctors counter a cancer’s defenses against chemo, helping ensure that even the most high-risk patients are able to beat the disease.
“If the cancer cells in a child try to evade chemotherapy by altering their cell surface, we can modify the targeted drug delivery system so it is able to recognise that altered cancer cell,” said Moles. “There will be no easy escape.”
We’d love to hear from you! If you have a comment about this article or if you have a tip for a future Freethink story, please email us at [email protected].