A rare but potent genetic mutation that alters a protein in the brain’s immune cells, known as microglia, can give people as much as a threefold greater risk of developing Alzheimer’s disease. A new study by researchers in The Picower Institute for Learning and Memory at MIT details how the mutation undermines microglia function, explaining how it seems to generate that higher risk.
“This TREM2 R47H/+ mutation is a pretty important risk factor for Alzheimer’s disease,” says study lead author Jay Penney, a former postdoc in the MIT lab of Picower Professor Li-Huei Tsai. Penney is now an incoming assistant professor at the University of Prince Edward Island. “This study adds clear evidence that microglia dysfunction contributes to Alzheimer’s disease risk.”
In the study in the journal GLIA, Tsai and Penney’s team shows that human microglia with the R47H/+ mutation in the TREM2 protein exhibit several deficits related to Alzheimer’s pathology. Mutant microglia are prone to inflammation, yet are worse at responding to neuron injury and less able to clear harmful debris, including the Alzheimer’s hallmark protein amyloid beta. And when the scientists transferred TREM2 mutant human microglia into the brains of mice, the mice suffered a significant decline in the number of synapses, or connections between their neurons, which can impair the circuits that enable brain functions such as memory.
The study is not the first to ask how the TREM2 R47H/+ mutation contributes to Alzheimer’s, but it may advance scientists’ emerging understanding, Penney says. Early studies suggested that the mutation simply robbed the protein of its function, but the new evidence paints a deeper and more nuanced picture. While the microglia do exhibit reduced debris clearance and injury response, they become overactive in other ways, such as their overzealous inflammation and synapse pruning.
“There is a partial loss of function, but also a gain of function for certain things,” Penney says.
Misbehaving microglia
Rather than rely on mouse models of TREM2 R47H/+ mutation, Penney, Tsai, and their co-authors focused their work on human microglia cell cultures. To do this they used a stem cell line derived from skin cells donated by a healthy 75-year-old woman. In some of the stem cells they then used CRISPR gene editing to insert the R47H/+ mutation and then cultured both edited and unedited stem cells to become microglia. This strategy gave them a supply of mutated microglia and healthy microglia, to act as experimental controls, that were otherwise genetically identical.
The team then looked to see how harboring the mutation affected each cell line’s expression of its genes. The scientists measured more than 1,000 differences, but an especially noticeable finding was that microglia with the mutation increased their expression of genes associated with inflammation and immune responses. Then, when they exposed microglia in culture to chemicals that simulate infection, the mutant microglia demonstrated a significantly more pronounced response than normal microglia, suggesting that the mutation makes microglia much more inflammation-prone.
In further experiments with the cells, the team exposed them to three kinds of the debris microglia typically clear away in the brain: myelin, synaptic proteins, and amyloid beta. The mutant microglia cleared less than the healthy ones.
Another job of microglia is to respond when cells, such as neurons, are injured. Penney and Tsai’s team co-cultured microglia and neurons and then zapped the neurons with a laser. For the next 90 minutes after the injury the team tracked the movement of surrounding microglia. Compared to normal microglia, those with the mutation proved less likely to head toward the injured cell.
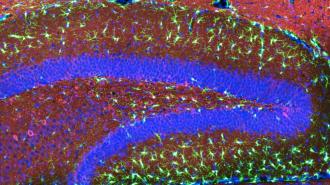
Finally, to test how the mutant microglia act in a living brain, the scientists transplanted mutant or healthy control microglia into mice in a memory-focused region of the brain called the hippocampus. The scientists then stained that region to highlight various proteins of interest. Having mutant or normal human microglia didn’t matter for some measures, but proteins associated with synapses were greatly reduced in mice where the mutated microglia were implanted.
What makes microglia tick?
By combining evidence from the gene expression measurements and the evidence from microglia function experiments, the researchers were able to formulate new ideas about what drives at least some of the microglial misbehavior. For instance, Penney and Tsai’s team noticed a decline in the expression of a “purinergic” receptor protein involving sensing neuronal injury, perhaps explaining why mutant microglia struggled with that task. They also noted that mice with the mutation overexpressed “complement” proteins used to tag synapses for removal. That might explain why mutant microglia were overzealous about clearing away synapses in the mice, Penney says, though increased inflammation might also cause that by harming neurons overall.
As the molecular mechanisms underlying microglial dysfunction become clearer, Penney says, drug developers will gain critical insights into ways to target the higher disease risk associated with the TREM2 R47H/+ mutation.
“Our findings highlight multiple effects of the TREM2 R47H/+ mutation likely to underlie its association with Alzheimer’s disease risk and suggest new nodes that could be exploited for therapeutic intervention,” the authors conclude.
In addition to Penney and Tsai, the paper’s other authors are William Ralvenius, Anjanet Loon, Oyku Cerit, Vishnu Dileep, Blerta Milo, Ping-Chieh Pao, and Hannah Woolf.
The Robert A. and Renee Belfer Family Foundation, The Cure Alzheimer’s Fund, the National Institutes of Health, The JPB Foundation, The Picower Institute for Learning and Memory, and the Human Frontier Science Program provided funding for the study.
Republished with permission of MIT News. Read the original article.