Australian researchers have found a way to reprogram cells from adults so that they’re more like embryonic stem cells. These memory-less cells can be reprogrammed to become any kind of cell, potentially unlocking an endless supply of stem cells for research or treatment.
Stem cells 101: Stem cells are capable of developing into any of the more than 200 types of specialized cells in your body, including muscle cells, brain cells, or heart cells.
This makes them incredibly useful to researchers. Scientists can study how stem cells become specialized to understand disease, or use them to create specialized treatments that can then be transplanted into people.
Embryonic stem cells are the gold standard for stem cell research.
The challenge: The supply of stem cells is limited. While people do have some stem cells in various parts of our bodies, adult stem cells can typically only turn into a handful of specialized cells, and they’re difficult for researchers to multiply.
Embryonic stem cells, which can be found in 3 to 5-day-old embryos, are the gold standard for stem cell research.
Scientists have to rely on people who’ve undergone in vitro fertilization procedures to donate their unused embryos to access those, though, and their use is controversial. They can also be rejected following transplants, since they don’t match the recipient’s DNA.
iPS cells can have abnormalities in their epigenomes that limit their use.
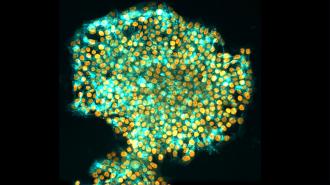
Fully specialized adult cells, such as skin cells, can be reprogrammed back into an embryonic-like state, creating what are known as “induced pluripotent stem” (iPS) cells. This means the person who receives the cells can be their own donor, which minimizes the risk of rejection.
However, iPS cells can have abnormalities in their epigenomes, the collection of chemical flags stuck onto DNA that determine which genes in a cell will be expressed — in some cases, it’s like the iPS cell has retained an epigenetic “memory” of its previous specialized state.
“This can create functional differences between the iPS cells and the [embryonic stem] cells they’re supposed to imitate, and specialized cells subsequently derived from them, which limits their use,” said lead researcher Ryan Lister from the University of Western Australia.
What’s new? Lister and his colleagues have developed a new technique, called “transient-naive-treatment” (TNT), which “resets” the cells’ epigenome during the reprogramming process — effectively wiping the “memory” of the iPS cells and making them more like embryonic stem cells.
“It solves problems associated with conventionally generated iPS cells.”
Jia Tan
To develop it, they studied what happens to the epigenome during the reprogramming process to see when abnormalities appeared. They then added a step to the process that mimics an epigenetic “reset” that happens naturally in embryos prior to implantation into the wall of the uterus.
According to the researchers, these iPS cells were able to differentiate into a variety of specialized cells better than ones created using the standard reprogramming method.
“It solves problems associated with conventionally generated iPS cells that if not addressed could have severely detrimental consequences for cell therapies in the long run,” said co-first author Jia Tan from Monash University.
Looking ahead: While more research is needed to better understand exactly what causes epigenetic abnormalities in iPS cells and how they’re corrected, the researchers are optimistic that their new reprogramming method will be a boon to stem cell research.
“We predict that TNT reprogramming will establish a new benchmark for cell therapies and biomedical research, and substantially advance their progress,” said Lister.
We’d love to hear from you! If you have a comment about this article or if you have a tip for a future Freethink story, please email us at tips@freethink.com.