A biotech startup hopes to transplant pig hearts from genetically engineered swine into young children with serious heart defects before the end of 2024.
The challenge: Right now, nearly 250 children under the age of 5 are on the US waiting list for a donor heart, and because of their small size, these would-be transplant recipients can’t accept hearts from adults — they have to wait for one from a comparably-sized child.
Due to the limited supply of such organs, an estimated 30% of children under 2 who are waiting for a donor heart will die before one becomes available.
“Pediatric patients have a greater clinical need, because there are far fewer other options available to them.”
Chris Gyngell
Pig hearts: Massachusetts-based biotech company eGenesis is working to end the global organ shortage by genetically engineering pig organs to be suitable for transplantation into humans, and it plans for some of its first recipients to be children under the age of 2 in need of new hearts.
“The fact is that pediatric patients have a greater clinical need, because there are far fewer other options available to them,” Chris Gyngell, a bioethicist at Murdoch Children’s Research Institute, who isn’t involved with eGenesis, told MIT Technology Review.
How it works: Doctors have been experimenting with xenotransplantation — the transplanting of animal organs and tissues into people — for centuries, and almost every attempt has ended with the patient’s body rejecting the organ almost immediately.
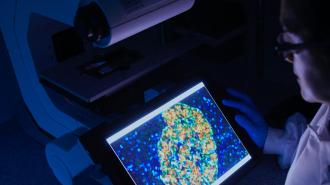
To minimize the chance of this happening with its pig hearts, eGenesis is using the gene-editing technology CRISPR to make more than 70 edits to the DNA of pigs.
Once the genetically engineered piglets grow to a suitable size, their organs can be harvested.
Some of the edits knockout pig genes that make proteins likely to trigger the human immune system, while others add human genes that eGenesis believes will help prevent organ rejection. Most, though, are designed to prevent ancient viruses, called endogenous retroviruses, that have hidden their DNA in the pigs’ genetic code from being able to replicate after the transplant.
eGenesis makes these edits to cells taken from a pig’s body. It then removes the nucleus from a pig egg cell and replaces it with the nucleus from an edited body cell. This process — somatic cell nuclear transfer — creates an embryo that can then be implanted into a surrogate sow.
Once the sow’s piglets are born and grow to a suitable size, their organs can be harvested.
The latest: eGenesis says it has created hundreds of genetically-modified pigs, some of which are now more than 4 years old. Its goal now is to be ready to transplant pig hearts into children under the age of 2 with serious heart defects, who cannot find a suitable human donor, before the end of 2024.
To prepare for that, it plans to transplant pig hearts into 12 infant baboons first.
“The first two are very encouraging from cardiac performance … the hearts look good.”
Mike Curtis
Two of those surgeries have happened so far, and in both cases, the animals died from surgical complications: the first within a day, due to a blocked IV, and the second after 9 days due to issues the surgeons faced connecting the baboon’s blood vessels to the pig heart.
Mike Curtis, eGenesis’ CEO and president, says the surgeons don’t expect to encounter the same surgical complications with future transplants, and the whole team was pleased with how the pig hearts themselves performed following the procedures.
“[In both cases], the heart itself was beating well,” Curtis told MIT Tech Review. “So far, the first two are very encouraging from cardiac performance … the hearts look good.”
The big picture: The performance of eGenesis’ pig hearts in the baby baboons is just the latest promising development in the world of xenotransplantation.
In January 2022, surgeons in Maryland transplanted a heart from a genetically engineered pig, created by the company Revivicor, into a man with end-stage heart failure who wasn’t able to receive a human transplant. He then lived for more than two months before dying due to a combination of factors.
Revivicor pig hearts have also been transplanted into two people who were brain dead and on life support. In both cases, the hearts performed well and showed no signs of rejection. The companies’ pig kidneys, meanwhile, have also performed well in a brain dead patient. (In all three cases, the studies ended with the patients being taken off life support after three days, as they originally would have been.)
eGenesis, meanwhile, recently published a paper detailing how 17 of 25 monkeys that received life-saving transplants of its gene-edited pig kidneys lived for at least 60 days. According to Curtis, some monkeys with the pig kidneys are still alive more than a year after the surgery.
Ultimately, after centuries of disappointing outcomes, it’s finally starting to look like xenotransplantation might actually be able to help end the organ shortage, for both adults and children.
We’d love to hear from you! If you have a comment about this article or if you have a tip for a future Freethink story, please email us at tips@freethink.com.