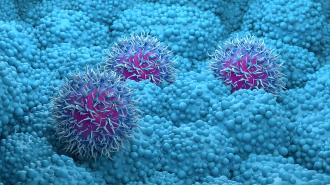
A discovery about how pancreatic cancer spreads could lead to better therapies for the hard-to-treat disease, which kills more than 50,000 people in the US every year. Researchers are already testing an existing drug, used for organ transplants, to stop the cancer’s spread.
The challenge: Pancreatic cancer is relatively rare, accounting for just 3% of cancers diagnosed in the US, but it’s notoriously hard to beat — 88% of patients die within five years of finding out that they have the disease.
A major reason for the low survival rate is that pancreatic cancer is hard to detect early, when treatments are most effective — patients often don’t experience symptoms until large tumors have formed or the cancer has metastasized, meaning it’s spread to other parts of the body.
Pancreatic cancer is relatively rare, but notoriously hard to beat.
Even when pancreatic cancer is found early, though, it’s still very difficult to treat.
“Pancreatic cancer cells are able to survive a lot of things — radiation therapy, chemotherapy, having no oxygen or blood supply,” said Arturo Loaiza-Bonilla from the Cancer Treatment Centers of America, who wasn’t involved in the new study. “They just survive for a long time.”
What’s new? Pancreatic cancer is caused by DNA mutations that trigger pancreas cells to grow out of control, but what causes the cancerous cells to spread beyond the pancreas isn’t well understood.
To find out more about that process, an international team of researchers analyzed about 400 samples of the most common type of pancreatic tumor (pancreatic ductal adenocarcinoma, or PDA).
“The disappearance of RBFOX2 protein … contributes to the invasive capabilities of the cancer cells.”
Rotem Karni
By comparing samples from metastatic and non-metastatic PDA tumors, they discovered that metastatic tumors contained far lower levels of a protein called RBFOX2, which plays a role in how RNA molecules are processed.
“Our unique findings demonstrate that the disappearance of RBFOX2 protein causes hundreds of genes to produce RNAs and proteins in a different way, which contributes to the invasive capabilities of the cancer cells,” said researcher Rotem Karni from the Hebrew University.
“We found that restoring RBFOX2 to PDA metastatic cells inhibits the formation of metastases, while the elimination of RBFOX2 in non-metastatic PDA cells stimulates the formation of pancreatic cancer metastases,” he continued.
“These findings offer two possible options for treatment of metastatic pancreatic cancer.”
Rotem Karni
Looking ahead: Once the researchers discovered the role of RBFOX2 in pancreatic cancer metastasis, they set out to see if they could use that information to stop the disease from spreading.
This led to the discovery that azathioprine, a drug typically administered to organ transplant recipients, could act on a group of genes affected by the disappearance of RBFOX2 in a way that delayed metastasis in mouse models.
The researchers also found that if they genetically altered metastatic cells from humans to express RBFOX2, the cells did not spread when transplanted into mice.
“These findings offer two possible options for treatment of metastatic pancreatic cancer: either a known drug that inhibits a process that is affected by RBFOX2, or an RNA-based therapy that intervenes in the processing of specific RBFOX2-affected RNAs,” said Karni.
“We are now talking with our collaborators in medical centers to convince them to start a clinical trial.”
Rotem Karni
While this research doesn’t address the problems of pancreatic cancer being hard to detect before it’s already metastasized, the ability to halt its spread once a patient is diagnosed could improve outcomes.
“[W]e are researchers, not clinicians, but we are now talking with our collaborators in medical centers to convince them to start a clinical trial with either azathioprine or similar drugs that are not yet approved,” Karni told the Times of Israel.
We’d love to hear from you! If you have a comment about this article or if you have a tip for a future Freethink story, please email us at tips@freethink.com.